What Is Antibiotic Resistance?
What are antibiotics?
Antibiotics are drugs that kill bacteria or inhibit their growth.
Antibiotics can be used to treat bacterial infections in people and animals.
Antibiotics are critical for treating all kinds of bacterial infections, and they make it possible to safely perform medical procedures and treatments ranging from caesarian section to chemotherapy for cancer patients.
What is antibiotic resistance?
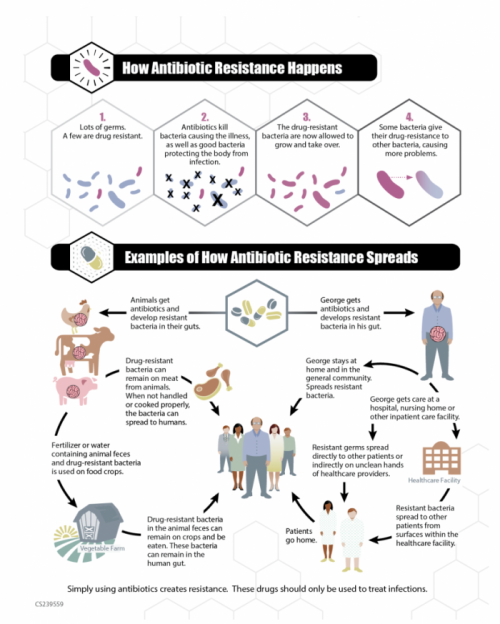
Antibiotic resistance happens when an antibiotic loses its ability to effectively control or kill bacteria. The bacteria become "resistant" and continue to grow because the antibiotic being administered has no ability to kill them. The World Health Organization, the U.S. Centers for Disease Control and Prevention and many other public health experts agree that we may soon be living in a world where antibiotics are no longer a match for drug-resistant bacteria, often called superbugs.
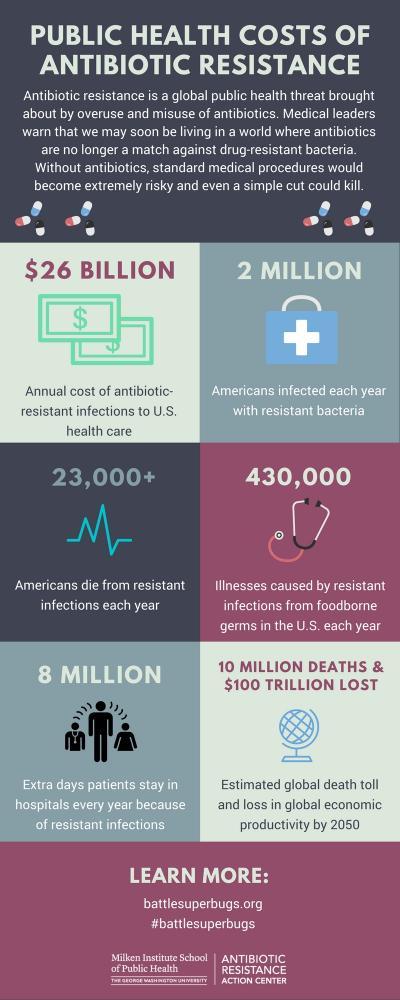
According to the CDC, over 2 million people every year become infected with bacteria that are resistant to antibiotics. At least 23,000 people die as a direct result of these infections every year.
Credit: Centers for Disease Control and Prevention
What is a superbug?
A superbug is a bacteria that has high levels of resistance to many different antibiotics.
How did we get in this situation?
Widespread antibiotic use in human medicine and livestock production has helped fuel the growth of antibiotic-resistant bacteria (aka superbugs).
Additionally, in the developing world, antibiotics are often sold without prescription and the lack of clean water and good sanitation helps superbugs spread among the population. Just as we are facing a major global crisis with antibiotics, pharmaceutical companies are shutting down their antibiotic development efforts in pursuit of more lucrative drugs.
What does a post-antibiotic future look like?
Today, tens of thousands of people in the U.S. die of antibiotic-resistant infections each year. As bacteria become increasingly resistant to antibiotics, even common infections – such as urinary tract infections – will be difficult to treat and can become life-threatening. In the next 30 years, antibiotic-resistant infections are expected to overtake cancer as the leading cause of death worldwide, and experts predict that based on current population estimates, could kill one person every three seconds.
Who is at risk of antibiotic-resistant infections?
Everyone is at risk of antibiotic-resistant infections, but those at the greatest risk for antibiotic-resistant infections are young children, cancer patients, and people over the age of 60.
Also at higher risk are patients who receive specialized care such as organ/bone marrow transplant, chemotherapy, complex surgeries and joint replacements, dialysis, as well as the elderly, children and premature infants and soldiers and veterans.
If trends continue, antibiotic-resistant infections are predicted to dramatically increase the death rates among women giving birth.
What are some consequences of antibiotic resistance?
The public health consequences of losing antibiotics are almost incomprehensible. Standard medical procedures would become extremely risky and even a simple cut could kill. In many cases, antibiotic-resistant infections lead to prolonged and/or costlier medical treatments; extended hospital or rehabilitation stays; additional doctor visits; and greater disability and death compared with infections that are easily treatable with antibiotics.
The annual costs of antibiotic-resistant infections in the U.S. range as high as $20 billion in direct healthcare costs, with additional costs to society for lost productivity as high as $35 billion a year.
Why should I be concerned about antibiotic use in food animals?
All uses of antibiotics contribute to the antibiotic resistance crisis we face. According to the most recent publicly available data, more than 35 million pounds of antibiotics are sold for use in food animal production every single year in the U.S. compared to 7 million pounds in human medicine.
The majority of the drugs used on industrial farms are to compensate for overcrowding and dirty living conditions, not to treat sick animals. Dangerous antibiotic-resistant bacteria spread from farms to people through direct contact with animals, farm runoff into waterways and on contaminated meat and poultry products.
What can be done to help slow the antibiotic resistance crisis?
- Use antibiotics more carefully in humans and animals to end the rise in antibiotic-resistant infections.
- Prevent infections, thus eliminating the need to treat them.
- Development of new antibiotics.
- Development and adoption of new tools to prevent the spread of antibiotic-resistant bacteria.
What can be done to stop overprescription of antibiotics in people and food animals?
A multi-pronged approach is necessary. Appropriate antibiotic use in people and food animals is essential. These drugs should be used when necessary, for the right dose and duration. Everyone has a role to play in reducing use.
What can you do?
- Ask when antibiotics are needed and not needed. Do not pressure your healthcare provider to prescribe medications but ask 'What can I do to feel better?' Ask when you should return if you do not get better or if your symptoms get worse.
- Take medication as prescribed. Take it exactly as directed, the entire course of medications, so there is none left over to “save.” Never take someone else’s medications and do not share antibiotics.
- Preventing illness in the first place is also important. Wash your hands, cover your cough and stay home when you are sick. Also, get your annual flu shot and any other vaccines recommended by your physician.